Limb/Knee transplants, also called knee arthroplasty, in which a knee is jostled with some new parts (ex, artificial bones) to help the person start movement again, and it is one of its types, so it is very easy to do it. The operation should involve not the knee-capping but the reconstruction of the cartilage and bone of the knee, which can be implanted with synthetic materials such as metal, plastic, or ceramics. It is usually suggested for those who suffer chronic knee pain that didn’t respond to nonsurgical treatments and are affected by osteoarthritis, rheumatoid arthritis, and other similar injuries.
There are over 850,000 knee replacements in the U.S. each year, and it’s an orthopedic testament to a new life for those who’ve been hobbled with knee problems. We want to tell you about knee transplants; here in this article, we will let you know the knee transplant procedure, type of transplant, benefits, side effects, recovery, and what to expect. This is a complete guideline for everyone who desires this life-saving transplant.
Also Read: Beat the Heat: Summer Health Tips for Everyone
What is Knee Transplantation?
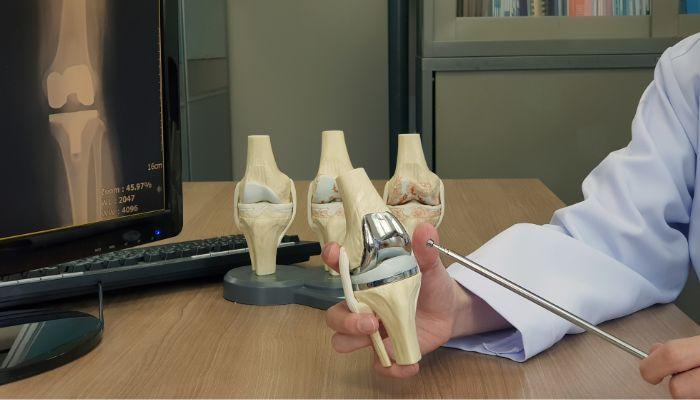
Arthroplasty (literally “surgical repair of joint”) is an orthopedic surgical procedure where the articular surface of a musculoskeletal joint is replaced, remodeled, or realigned. The knee is a large complex hinge joint that includes the femur (thighbone), tibia (shinbone), and patella (kneecap) cartilage, ligaments, and tendons that are the soft form of tissue also help to move & stabilize it easily. Without the cartilage – worn away by arthritis or some other injury the bones rub together, and people suffer pain and stiffness or lose the function of the joint.
A knee transplant is a procedure in which a surgeon removes the damaged cartilage and bone and replaces it with an implant that mimics the function of a typical knee. These components include:
- Femoral Component: A metal or ceramic that covers the end of the thigh bone.
- Tibial Component: A metal and plastic part that goes over the top of the shin bone.
- Patellar Component: A plastic implant that covers the bottom of the kneecap (May or may not be used, depending on the procedure).
- Plastic Spacer: An inner liner material between femoral and tibial components for low friction sliding.
The intent is to help relieve pain, restore function and improve the patient’s overall quality of life. A knee transplant is offered for those patients whose pain and discomfort are not treated by conservative measures (for example, physical therapy, medications, or injections).
Types of Knee Transplantation
There are two main kinds of knee replacement, which are designed for the severity of knee damage and what the patient needs:
1. Total Knee Replacement
The most frequent kind, TKR, replaces all three compartments of the knee joint: the medial (inside), lateral (outside), and patellofemoral (under the kneecap). It is best for arthritis patients who have multiple joint involvement or joint destruction. TKR is a very successful procedure with more than 90% of implants surviving for 15–20 years.
2. Partial Knee Replacement
This type of operation, also called unicompartmental knee replacement, PKR, is performed when only the single compartment of the knee is damaged, and the other compartments are healthy (usually the other two compartments). It is more of a minor operation. Anyway, less invasive / smaller incision / faster recovery. However, PKR is only appropriate for around 10–25% of patients with localized damage, and, in some cases, it may not be as effective at easing pain as TKR.
Specialised procedures such as Osteochondral Allograft Transplantation (OCA) or Autograft Transplantation (OAT) can also be helpful in young people with localised cartilage defects. These include transplanting harvested cartilage and bone tissue from a donor (allograft) or the patient’s own body (autograft) to repair localized defects and to protect the joint for longer before it needs to be replaced entirely.
Who Needs Knee Transplantation?
A knee transplant is usually for those who are:
- Unbearable Pain: Pain is so severe that you can’t do your day-to-day tasks, like walking upstairs, walking, and sleeping.
- Limited Mobility: Lack of normal knee movement and inability to perform ordinary activities due to just one knee being stiff or unstable.
- Arthritis: Cartilage wear is the result of osteoarthrosis, rheumatoid arthritis, and post-traumatic arthritis.
- Failed Non-surgical Treatments: If medications, physical therapy, injections, or changes to your lifestyle have not provided relief.
- Knee Deformities: Structural problems, like bowlegs or knock-knees, resulting from joint damage.
The process is primarily an option for individuals over the age of 60. However, younger patients who have severe knee damage can also be considered. However, younger patients can have wear to implants as a function of time, leading to some requirements later on.
The Knee Transplantation Procedure
The surgery of knee transplantation is an established surgery with a duration of operation generally that ranges from 1 to 3 hours. Here’s an explanation, step by step:
1. Preoperative Evaluation
The orthopedic surgeon reviews your past medical history, performs a physical exam, and may order X-rays or MRI to assess the degree of damage to the knee before deciding whether to proceed with surgery. Blood test, along with other diagnostics, confirms the patient is in good condition for surgery.
2. Anesthesia
It is done under general anesthesia (the patient is put to sleep) or regional anesthesia (such as spinal or epidural, numbing the lower body). Patients can also be given sedatives for their comfort.
3. Incision and Joint Exposure
An 8 – 10-inch incision (although there are some minimally invasive techniques with smaller incisions) is made over the knee to reach the joint. Muscles, tendons, and ligaments are gently retracted.
4. Bone Reshaping
Badly worn cartilage and bone from the femur, tibia, and, occasionally, the patella are scraped away with specially designed instruments. The bone deflections are matched to the prosthesis components.
5. Implant Placement
The metal and plastic parts are fitted onto the prepared ends of the bones and fixed into place with or without bone cement. The parts are put together with a plastic spacer that allows for a sliding motion.
6. Testing and Adjustments
Alignment, stability, and range of motion of the knee are evaluated. It will be optimized during the maintenance for smooth function.
7. Wound Closure
The wound is closed with stitches or staples and a sterile dressing is applied.
8. Postoperative Care
Patients are transferred to a recovery area, where pain management and physical therapy are initiated. Most of the patients are discharged home the same day (outpatient surgery) or are in the hospital for 1-2 days.
More advanced procedures are now performed in a minimally invasive fashion using robotic technology or augmented reality to enhance precision and outcomes.
Benefits of Knee Transplantation

Transplantation of the knee brings multiple advantages and makes a difference in the patients’ lives:
- Pain Relief
The operation replaces arthritic joint surfaces, resulting in freedom from chronic pain and allowing patients to conduct normal daily activities without any pain. - Improved Mobility
Patients will once again be able to walk, climb stairs, and do low-impact activities (such as playing golf or swimming), which leads to an improved level of independence. - Enhanced Quality of Life
Decreased pain and enhanced function allow patients to join in social and recreational activities with a resultant enhancement in overall quality of life. - Long-Term Durability
More than 90% of knee implants last 15 to 20 years, with some lasting 25 years or more, delivering long-term relief. - High Success Rate
Knee transplant is successful, greater than 90%, and most patients show significant reduction of pain and functional improvement.
Risks and Complications
knee transplantation is safe, but it does have risks:
- Infection: Infection (less than 2% of cases but can be severe, especially in immunocompromised patients, e.g., past solid organ transplant).
- Blood Clots: Blood Clots, Deep vein thrombosis, or, in some cases, pulmonary embolism is a risk, which one way to mitigate is by using blood thinners and getting people up and moving early.
- Implant Complications: The implant may loosen or wear out and result in revision surgery.
- Stiffness or Reduced Range of Motion: Scar tissue or poor rehabilitation may cause restriction of knee motion.
- Nerve or Blood Vessel Damage: At surgery, it is rare but definitive.
- Periprosthetic Fractures: Fractures that occur around the implant and are more frequent for people whose bones aren’t strong.
Patients with solid organ recipients are associated with high complication rates (22.58%) and more infections (6.99%) secondary to immunosuppressive drugs.
Also Read: Top 10 Surgeons In India: Your Complete Guide To The Best Specialists In Every Field
Recovery and Rehabilitation
Knee replacement recovery normally takes 4 months to a year, depending on the patient’s health, age, and rehabilitative compliance. Key aspects include:
- Early Postoperative Phase
They began moving the knee on the day after surgery, and were frequently treated with a continuous passive motion (CPM) device to prevent stiffness. I Unraveling There are no drugs, just medications and regional nerve blocks for pain. - Hospital Stay
Most patients are discharged within 0–2 days. A few may need to spend a brief time in a rehabilitation facility. - Physical Therapy
A gradual rehabilitation program to improve the strength, flexibility, and range of motion is recommended. Exercises like walking, lifting the legs, and bending the knees. Patients usually spend the first weeks and months after surgery using a walker or cane. - Long-Term Recovery
Complete recovery can take a year, but most individuals can return to normal activities in 3 to 6 months. Low-impact sports, such as swimming or cycling, are advised, although high-impact contact sports, such as running, are generally not. - Follow-Up Care
The patient should have regular appointments with the surgeon to make sure the implant is in good condition. Patients also do not want to wait too long to realize the benefits of surgery, nor do they want to have the surgery too early, as more load leads to more revision in younger patients.
Alternatives to Knee Transplantation
For patients who are unwilling or unsuited to knee replacement, options include:
- Nonsurgical Treatments: Physical therapy, Nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroid injections, or hyaluronic acid injections.
- Genicular Artery Embolization (GAE): A non-surgical treatment for pain relief in which blood supply to nerves that cause pain is cut off.
- Neuromodulation: A method to stop pain signals by reattaching sensory nerves to motor nerves, decreasing the pain without replacing the joint.
- Cartilage Repair Techniques: Cartilage Repair -Microfracture, autologous chondrocyte implantation (ACI), or osteochondral autograft/allograft transplantation for focal cartilage defects, especially in younger patients.
Preparing for Knee Transplantation
Patients must take following precautions for a successful das-phase of treatment:
- Muscle Strengthening: Practice light workouts such as walking or swimming before your surgery to help with the recovery process.
- Set up the Home: Make sure remote controls and medications are within reach and food is on hand to prepare easily.
- Set Up Support: Ask a friend or loved one to help with everyday activities and driving after surgery.
- Participate in Pre-operative Evaluation: Take all relevant tests and talk through expectations with the surgeon.
The Future of Knee Transplantation
Advancements in knee transplantation are improving outcomes and expanding options:
- Robotic-Assisted Surgery: Adds precision during implant placement and minimizes recovery and complications.
- Augmented Reality: Helps surgeons see the knee in real-time, enhancing precision.
- Advanced Implants: New materials and designs, such as the CartiHeal Agili-C implant, spur on cartilage regrowth and postpone the necessity for complete replacement. Other options have emerged.
- Biologic Therapies: Research is ongoing in the use of stem cell treatments or bone marrow aspirate concentrate (BMAC) to improve graft integration and healing.
Conclusion
Knee replacement, or knee arthroplasty, is an excellent option for those who suffer from chronic knee pain and limited function due to arthritis and injury. It has an over 90% success rate and patients are still experiencing pain relief 5 – 6 years after the implant and are seeing increased mobility and quality of life. Although complications such as infection or implant wear do occur, advances in surgical procedures and rehabilitation programs have resulted in improving outcomes as time goes on.
Patients who are considering a knee abortion must consult an experienced orthopedic surgeon who can explain the procedure and reasons and expectations. Most patients can get back to an active, pain-free life when prepared and rehabbed correctly, making the knee transplant an exciting new option for people with severely damaged knees.